February 1, 2005
Case Study
Recently a friend and former patient of mine asked me over to talk to her about some progressive symptoms that she had been experiencing over the last several months. She had first noticed that occasionally she would lurch from one wall to the other while walking down a hallway. As these episodes continued, she also began to notice that if she closed her eyes in the shower she would become disoriented and lose her balance.
In fact, she had taken a few nasty falls in the last several months, one of which had occurred at night, something that had never happened to her before.
Additionally, she was noticing that when she worked in the garden while in a squatting position, if she leaned over just a little too much, without any warning, she would find herself on the ground. Further yet, she was now experiencing some difficulty with her handwriting and occasionally even with her speech. During the discussion her elderly husband commented that he had noticed of late that her driving was becoming a bit erratic in that she now seemed to hug the right side of the lane in traffic and any needed minor adjustment of the steering wheel seemed to result in her weaving as well.
Due to this progressive disability, my friend and her husband had had to abandon their business which had required some physical labor. She was also planning to hire out much of the work that she used to do herself around the house and because of this she and her husband were seriously considering selling their home and moving to a condo.
When I encountered all of these symptoms it became clear to me that her difficulties stemmed from some sort of dysfunction of the neuromuscular system. But exactly what and where was her problem? The various possibilities flooded through my mind as I reviewed her multiple symptoms. The analysis that a physician mentally goes through at times like this usually results in the formulation of a differential diagnoses; which consists of the most likely possible diagnoses that could explain the patient’s com-bination of symptoms. Each one is considered and various questions are asked of the patient and a specific examination is done in order to determine if she has any other symptoms or signs that would be consistent with each of the diagnoses being considered. After completing a history and a physical examination, the physician can often make a tentative diagnosis followed by a short list of other possible causes based on the patient’s presentation and the physician’s understanding of the pathophysiology of human disease.
I have always marveled at how similar the mental processes of my profession are to those of an auto mechanic. They too must do a diagnostic analysis to determine what may be wrong with your car. If it won’t start one has to consider among other things; a dead battery, a defective starter, no gas in the gas tank, and a blocked fuel line etc.
Back to Basics
An overview of neuromuscular function, at the biomolecular and electrophysiological levels, has already been discussed in three of my prior columns. (Wired for Much for More than Sound Parts I, II, & III). Together, they explain how after a neuron is appropriately stimulated it is capable of sending a message by way of neurotransmitters, either to other neurons for the purpose of providing information for analysis, or to muscle cells to tell them what to do. If you aren’t familiar with the underlying complexity of nerve and muscle cell function, or you need a refresher course, I would suggest that you consider reading these three articles now before you continue since what I will be describing from here on will largely consist of the “macro” aspect of neuromuscular function. It’s important that you have a clear understanding of what is behind all of the messages that are being sent this way and that in order to allow us to perform the activities of life.
Whenever I’ve encountered criticism to the questions and conclusions that I logically derive from the information that I provide in my column, I am always amazed to find that the critic simply assumes that the possibility of a particular set of biomolecules existing in the human genome in and of itself allows for proper function. It takes much more than that. Having the right biomolecules available is only the beginning. The body must also have the capacity to produce and control the amounts of these biomolecules, which is usually accomplished by a negative feedback system often consisting of a sensor that detects a certain biochemical parameter that is vital for life. In the case of the neuro-muscular system, it must know what to do with the information provided in order for proper function that allows for survival to take place. That’s why I think it’s important for you to be intimately aware of how every aspect of a particular human physiological function takes place, and just as importantly, how even a minor defect can result in dysfunction, disability and often death. For remember, while our hominid ancestors were busy fighting the battle of natural selection, they did not have the luxury of modern medical science and the socioeconomic programs of today to give them succor and support when things broke down.
One muscle and nerve cell acting on their own are incapable of performing the activities that our bodies must be able to do for survival on earth. Just imagine a primitive hominid trying to catch prey for food or evading an aggressor. It is possible to visualize in our mind’s eye his sleek body darting this way and that, first stopping and then starting again, as his neuromuscular system responds to the needs at hand. Certainly it is self-evident that without an intact and properly functioning neuromuscular system, the chances of our hominid ancestors being able to survive the battle of natural selection would be small, in fact they would be non-existent.
Let’s look into medical science’s understanding of how our bodies are able to run and do all sorts of other things that enrich our lives and that at the same time allowed our hominid ancestors to survive on earth. Along the way we’ll consider and apply what we encounter to the differential diagnoses that apply to my friend’s neurological condition and in so doing try to come up with a provisional or working diagnosis that may explain her problem.
Move it Buddy
I think that the best place for you to start is for you to get out of your chair right now and try testing out your neuromuscular system yourself. Take a few strides back and forth. Go sideways, backwards and spin around. Do a jig. Concentrate on what your body must be able to do in order for you to accomplish these actions. Changes in direction require that your body’s neuromuscular system must be able to know where it sits in space and its rotational and linear relationship with its surroundings. Think about what sensory features of the body must be active during these movements. Only after this has been determined can the nervous system then send out the proper instructions to its muscles to tell them what to do in order to react properly. Consider the muscles that you are using in the arms, your legs, and particularly the spine, in order to be able to move around like this and maintain your balance on two narrow feet.
In short, the ability to walk and run is dependent on much more than just the obvious muscles used for mobility. It requires a lot of sensory input that is constantly being integrated and interpreted in the higher levels of the nervous system, and the use of a lot of other skeletal muscles throughout the body that we don’t usually associate with this activity. Voluntary coordinated purposeful movement is absolutely necessary for human survival. It consists of maintaining posture, or position, in space while at the same time allowing for goal-directed activity to take place. Let’s look at what is required of the neuromuscular system for it to achieve this function while at the same time considering how each of the components that are necessary may or may not be related to my friend’s diagnostic dilemma.
Sensory Reconnaissance
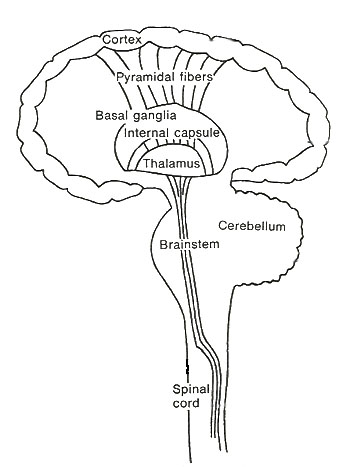
It is known that any interruption or dysfunction of the sensory pathways that are responsible for feeding information to the neuromuscular system will result in impairment of voluntary coordinated purposeful movement. Remember, you can’t give commands about an operation unless you have information about what is going on out there. The sensory organs of the body together provide it with an intelligence retrieval system. What happens to these messages and how they ultimately result in the execution of a particular action is as yet poorly understood. However it is known that sensory messages travel into the spinal column, or brain stem, where they are passed on to other regions of the brain, such as the thalamus, the basal ganglia, the cerebellum, and the motor cortex of the cerebrum for analysis and processing. (see Figure 1) Some of the necessary sensory input which we’ll discuss below includes: vision, balance, joint position, muscle tension, pain, vibration, pressure, temperature, and fine touch. Just think about what could happen to your ability to coordinate neuromuscular activity if any of these sensations were missing. Think about how it could have affected our hominid ancestors as they tried to catch prey or evade predators.
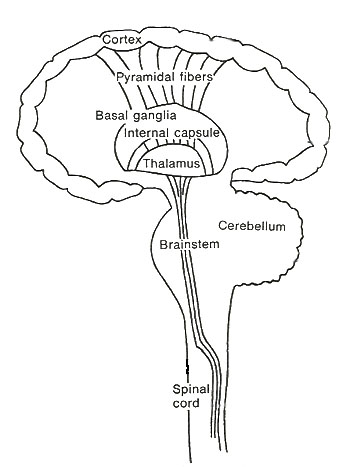
Figure 1. Basic setup for central nervous system.
Play it again Sam
The best way to consider these situations is to go through the exercise that we just did a few minutes ago. Stand up and stride back and forth and then go sideways and turn around. Do a jig again. While you do this try to make yourself aware of the sensory apparatus that you are using.
Blindfolded
Now try it all with your eyes closed. A little more difficult isn’t it? That’s because the eyes provide visual cues that help in coordinated muscular activity to maintain posture and to perform goal-directed actions. A detailed description and analysis of vision has been provided in three previous columns that I have dubbed as my vision trilogy. (Wired for Much More than Sound Parts IV, V & VI). For those who have not read these articles, or need an update on their understanding of how vision actually takes place, please refer to these columns to get an idea of its incredible complexity. Now one can see that vision also plays a major role in proper neuromuscular function. It’s hard enough to believe what evolutionary biologists propose to be the explanation for how human vision came into being, never mind considering that the neuromuscular system must somehow know what to do with this information in order to provide the body with a function that allows for survival.
Now, remember that my friend tended to lose her balance in the shower when she closed her eyes and that she had taken some nasty falls, one of which had occurred at night. She didn’t describe any visual problems but her symptoms were aggravated by her not allowing her neuromuscular system to have the benefit of those visual cues. In other words, whatever dysfunction she was having in her neuromuscular system was likely being at least partially compensated for by the use of visual cues whose loss made her neuromuscular system decompensate resulting in her loss of balance.
Closing her eyes made her problem worse because now the neuromuscular system was totally dependent on other sources of sensory information. Information that it was evidently having problems analyzing and coordinating with other input in a timely manner to prevent the loss of balance, sometimes resulting in a fall. The fact that my friend is experiencing this problem points, not to a visual abnormality, but to a problem somewhere else in the neuromuscular system. So let’s carry on.
Balancing Act
While whirling around I’m sure that you felt a bit of dizziness take hold. This would have been the vestibular apparatus in each ear letting you know about your motion in space. The faster you twirl around the stronger the sensation. But in addition to rotational acceleration, the vestibular apparatus is also able to detect linear movement such as the effects of gravity on the position of the body.
The vestibular apparatus is housed in the ear and consists of two chambers called the utricle and the saccule, and the three semicircular canals, all of which contain endolymph. (see Figure. 2). The utricle and saccule provide the body with information about the position of the head with respect to gravity and the semicircular canals are positioned in such a way as to notify the nervous system of any angular motion of the head.

Figure 2.
The information from the utricle and the saccule is important for the body’s ability to maintain its posture and the semicircular canals’ information is used to reflexively control eye movements to stabilize the retinal image. In fact, people with vestibular dysfunction have difficulty walking blindfolded over irregular surfaces and even when their eyes are open they often have problems walking because the retinal image keeps moving up and down rather than remaining stable. Just consider it. Without the brain’s ability to detect the angular motion of the head as it moves in any direction, which invariably occurs with almost any activity, it would not be able to stabilize the retinal image that it is at the same time receiving from the optic nerves
Try it yourself right now and see. Sit absolutely still and focus your eyes on a point far away. Imagine that this is something that you are pursuing in order to provide food for yourself and your family. Now, while still focusing on this object, move your head sideways and up and down. The ability to keep focusing on a particular point is dependent on your visual apparatus being able to direct the light to your fovea. But your ability to continue to be able to focus on it while you are in motion is dependent on the messages that the vestibular apparatus in your ears send to the brain, which then reflexively compensates by moving your eyes to keep the object of interest in focus.
Now, stand in front of a mirror and focus on your eyes. Turn your head sideways, up and down and even at angles, and you’ll see what I mean is happening. Move faster and faster in all directions. You cannot consciously tell your brain to compensate for this head motion yourself. It does it automatically by virtue of your decision to focus on something of interest. Certainly, one could allow one’s eyes to move at random with head motion by purposely not focusing on a particular object, but what purpose would this serve? All of human experience tells us that in order to be able to accomplish the task of survival, we must have the ability to maintain our focus on an object while we still remain in motion. This lesson in human neurophysiology shows that just having the sensory apparatus for vision, in and of itself, will not accomplish this necessity for human survival on earth.
The underlying mechanism for vestibular nerve stimulation by the utricle, the saccule, and the semicircular canals, is in many ways similar to the one in the cochlea of the ear, for hearing. (please see my last column on the ear and hearing; Wired for Much More than Sound Part VII). The sensory organs involved contain specifically oriented hair cells, whose stereocilia that project into the endolymph of the chamber involved, are bent with certain movements of the head. This results in the opening of K+ ion conduction channels, and since endolymph is high in K+ ions, (the only extracellular fluid in the body that has this very unique property), K+ ions rush in across the cell membrane, depolarizing the cell. This causes voltage-gated Ca++ ion channels to open, allowing Ca++ ions into the hair cell. The elevation of Ca++ ions in the hair cell causes the release of a neurotransmitter that then stimulates a nearby vestibular neuron.
Movement of the hair cell in the opposite direction will close the K+ ion transduction channels thereby inhibiting vestibular nerve discharge. The vestibular nerve, like the auditory nerve for hearing, has a basal level of activity which tells the brain that it is in “rest” mode. Any motion of the head that causes the above reactions to occur results in a modulation of vestibular nerve output that is then interpreted and integrated into the neuromuscular system.
Both the complex nature of the vestibular apparatus and the ability of the central nervous system to properly use this information to allow for mobility and survival need to be explained by evolutionary biologists. Simply comparing the structures of various organisms of differing sophistication without explaining where the more primitive ones came from in the first place, what genetic mutations could practically have resulted in the existence of these more advanced ones, and how each successive organism’s neuro-muscular system knew what to do with this new information to allow for functional survival, would, for most inquiring minds, seem to be inadequate.
A case in point is what we’ve just discovered in this lesson; the intimate relationship between vestibular and visual function that allows for survival that requires mobility. Both of these functions are dependent on end-organs (the vestibular apparatus located in the ears, and vision from the eyes) that are immensely complex at the gross anatomy, microscopic, biomolecular, and electrophysiological levels. But in addition to this, it is the central nervous system that must be able to take the nerve messages from these end-organs and process them in a way that allows it to know what to do in a given situation. Our present knowledge of how the system works shows that if most of what we know about it didn’t work properly, or were absent, then the whole system would be dysfunctional, and survival on earth would be severely compromised to say the least. But of course, that still leaves out most of what we don’t know about it, doesn’t it?
Pondering my friend’s complaints, one remembers that she did have problems with balance and had become disoriented when she closed her eyes in the shower. Could she have a vestibular problem? Maybe she has something wrong with the vestibular apparatus in the ear, the vestibular nerve, or the part of the brain that coordinates these messages? Conditions that could cause this include; an inflammation of the vestibular apparatus (labyrinthitis) or the vestibular nerve (vestibular neuronitis), benign positional vertigo (usually manifesting as severe vertigo with minimal head movement) which is a condition of the vestibular apparatus in the ear, or a tumor that is gradually growing and pressing on either the vestibular nerve or the brainstem. These are all things to keep in mind as we continue to do our analysis of her differential diagnosis. I’d say that a vestibular problem would be high on my list of possible diagnostic possibilities.
Sensory Deprivation ?
When you were striding back and forth and spinning around, did you notice what other sensory apparatus, besides vision and balance, were needed for you to perform these maneuvers? Although pain and temperature perception can prevent injury, and light touch and vibration sense have their own inherent uses, it is largely the pressure sensors in the feet, and the proprioceptors (muscle and joint sensors) throughout the legs and arms, and especially the neck and spinal column, that provide the necessary information to allow your neuromuscular system to keep you moving and staying balanced. The input from the pressure sensors of the feet help the nervous system to know what the distribution of the body’s weight is with respect to its center of gravity. And between the eyes, the vestibular apparatus, and the proprioceptors of the neck and spinal column, the brain becomes informed about where the head is sitting in its environment. All of this information is necessary in order for the neuromuscular system to perform its job properly and allow you to be able to survive on earth.
Now don’t forget, that each of these sensations that I’ve mentioned above have their own specific sensor that allows for the detection of that particular sensation. Pain is detected by naked nerve endings, but touch, pressure, warmth, cold, vibration and proprioception are tended to by such things as Meissner’s corpuscles, Pacinian corpuscles, Ruffini’s end organs, Krause’s end bulbs, Merkel’s disks, muscle spindles, and Golgi tendon organs (the latter two will be discussed in more detail in next month’s column).
Each of these sensory receptors responds to a particular physical force that affects our body by converting it into an electrical signal that is passed on to be interpreted by the nervous system. This process is called sensory transduction. If you recall your neuron electrophysiology, you’ll remember that the physical force that is being detected causes the specific sensory receptor cell to depolarize by opening up certain ion channels on the cell membrane. The resulting wave of depolarization travels down the neuron where it causes voltage-gated Ca++ ion channels to open up, letting in Ca++ ions. This influx of Ca++ ions signals the neuron to release neurotransmitters into the synapse between it and another neuron which is then further stimulated and the message is eventually passed on to the central nervous system for interpretation and analysis.
Where these numerous, well placed, sensory receptors came from, and how their information became integrated into the nervous system to allow for adequate survival function, would certainly seem to need some in-depth explanation by evolutionary biologists to verify the theory of macroevolution. An explanation that goes far beyond just comparing the nervous systems of more primitive organisms with our own. What is needed is a full understanding of how the primitive systems developed de novo, what mutations were necessary to produce the structures for a step-by-step development toward our own system, and finally, a thorough explanation of how the nervous system, consisting of over ten billion neurons in the central nervous system alone, is capable of what it does, namely; interpreting, integrating, and commanding action where and when it is necessary to do so, none of which is currently understood. For without this capability, a multi-system organism with a complex body plan would not be able to survive.
Two examples of medical conditions that can impair sensory perception resulting in a person having difficulty maintaining their balance, particularly when their eyes are closed are: sensory (peripheral) neuropathy, commonly seen in long-standing diabetes mellitus in which sensory nerve function is diminished or absent; and subacute combined degeneration due to Vitamin B12 deficiency which results in the degeneration of the spinal cord tract that carries some of these messages up to the brain.
Usually people with diabetic sensory (peripheral) neuropathy will experience some sort of tingling or other abnormal sensations in the toes, and even the fingers, long before their balance is affected. Although infrequently, people just aren’t aware of what’s been happening to them and sudden losses of balance and falls can sometimes be the first sign that someone has a sensory neuropathy. People with prolonged sensory deficiency often end up with something called Charcot joints, which have been grossly damaged because of the lack of the ability of the person to protect their joints from injury. My friend is not diabetic, she had not experienced any abnormal sensations in her hands or feet, and she had normal sensation on physical examination.
People with subacute combined degeneration of one of the sensory columns of the spinal cord usually cannot detect joint movements and vibration and they often have pernicious anemia from Vitamin B12 deficiency. However, my friend had no difficulty with these sensory tests and overall she feels very well. So it would appear that she is not suffering from this problem either.
Recap
So far we’ve only discussed the sensory component of neuromuscular function that allows us to run and jump, spin around, and remain active in our surroundings. One can readily see what our hominid ancestors would have needed to have possessed in order to survive on earth. Reviewing the case study, it would appear that the most likely diagnosis to consider from the sensory realm of things would be something in the order of a vestibular problem. It is still possible that my friend may have some other sensory problem involving the peripheral nerves or the pathways up to the brain that I wasn’t able to detect based on her history and physical examination, but this is less likely. Now we need to move on and look at the problem from the motor side. But I’ll leave that until next month so that you can go over everything here again. Then we’ll be looking at:
Wired for Much More than Sound Part IX--Run for your Life Part 2.
Dr. G.
Howard Glicksman M. D. graduated from the University of Toronto in 1978. He practiced primary care medicine for almost 25 yrs in Oakville, Ontario and Spring Hill, Florida. He recently left his private practice and has started to practice palliative medicine for a Hospice organization in his community. He has a special interest in how the ethos of our culture has been influenced by modern science’s understanding and promotion of what it means to be a human being.
Copyright 2004 Dr. Howard Glicksman. All rights reserved. International
copyright secured.
File Date: 1.01.05