April 1, 2005
Last month we started to look at the complexity of neuromuscular function by first considering the case of a friend of mine. If you recall, she had first noticed herself occasionally lurching against the wall as she would walk down a hallway. Later she began to experience more problems with her balance in that she would become disoriented in the shower on closing her eyes and she had had some pretty nasty falls resulting in injury. Finally, she had recently noticed that she was having some difficulty with her handwriting, her speech, and her ability to control her car in its lane of traffic.
I had asked you to go through some maneuvers that I had hoped would make you aware of what sorts of information and capabilities the neuromuscular system must have in order to allow us to do what we do. Last month’s column reviewed some of the sensory input that the neuromuscular system needs in order to be able to function properly. You can’t give commands that will be functionally effective if you don’t know where you are in space and what you’re up against in the surrounding environment.
In summary, we determined that there are various sensory apparatus, particularly; vision, vestibular function, proprioception, and pressure sense, that each play an important role in informing the central nervous system of what’s going on inside and outside the body thereby enabling it to decide what orders to give the motor system. After reviewing all of this and comparing it with my friend’s symptoms and signs, we concluded that if there were a dysfunction within one of the sensory apparatus that was at least partially or wholly responsible for her problem, that most likely it would be the vestibular system.
And if the vestibular system were not working properly, the specific areas to look at would be either the vestibular apparatus in the ears, the vestibular nerves, or the area in the brainstem that is responsible for vestibular function.
Muscle Make-up
Once the mind decides what it wants to do, how does it go about doing it? For the many people who believe in the theory of macroevolution, it would appear that for them, by simply stating that the neuromuscular system which has developed from more primitive ones, accomplishes what is needed, would seem to be sufficient, without accounting for its complexity. However, the devil is in the details. For one muscle cell does not a muscle make and coordinated muscular activity that allows for human survival is dependent on a whole host of components, about most of which neuroscientists know very little except to say what happens when things go awry. For as most people who seek understanding will tell you; “the more you learn, the less you know” which results in one having to have faith in the information and conclusions, particularly about origin, provided by others who are perceived as being the authorities on the subject.
Each skeletal muscle consists of many individual muscle fibers. These muscle fibers are the basic units of muscle tissue just as the neuron is the basic unit of nervous tissue. So just as a nerve consists of numerous neurons, each muscle similarly consists of individual muscle cell fibers that are joined together in a parallel fashion that together run the length of the muscle.
Remember that skeletal muscle is under direct nervous control and therefore it will not contract when needed to unless it is stimulated by the motor neuron that is associated with it. These motor neurons stimulate more than one muscle fiber at a time and therefore a message originating from the brain often ends up causing many muscle fibers to contract in order for the desired effect to take place. The motor unit consists of each motor neuron and the muscle fibers that it stimulates by way of releasing the neurotransmitter acetylcholine. (For a detailed description of the biomolecular and electrophysiological basis of nerve and muscle activity please see my prior three columns; Wired for Much More than Sound Parts I, II, and III. Only by understanding the incredible complexity of neuromuscular function, at its most basic level, can one then even begin to consider how it might have come into existence).
The number of muscle fibers controlled by any given motor neuron depends on the muscle and the activity required. For fine precise movements in the hand or the eye, there may be less than ten muscle fibers in a motor unit. But for coarse, strong movements, such as in the muscles of the back and legs, there may be several hundred. Each muscle consists of many motor units. Their combined, coordinated contraction, as directed by the nervous system, is what allows for muscle function and our ability to move about on earth.
So part of the answer of how muscles are able to move us around is that motor neurons pass on their messages to multiple muscle fibers which are all combined in one particular muscle so that their contraction is coordinated and generates enough power to allow us to do what we need to do.
Getting the Message Out
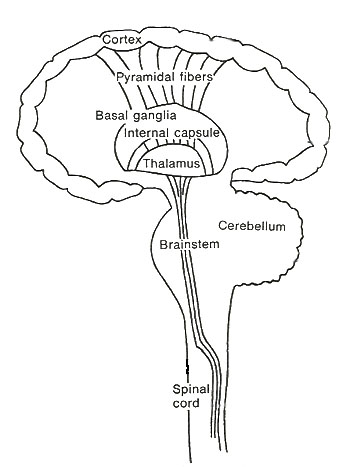
In a similar fashion to how sensory messages must pass up the spinal cord into the brain so that it has some information about what is going on in the body and its environment, motor messages that will ultimately result in muscle contraction and the body doing something, must pass down from the brain into the spinal cord as well.(Figure 1)
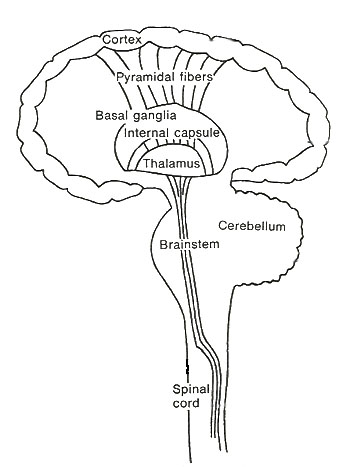
Figure 1. Basic setup for central nervous system.
From here the message reaches the motor neuron which exits the spinal cord and joins up with other motor neurons to become the motor component within a large peripheral nerve that carries the message directly to the muscle tissue. Here’s an example of how it all works.
Consider the event where someone is tickling your left foot and after several seconds you decide to pull your foot away. Sensory organs in your left foot are depolarized by the tickling and they send sensory nerve messages along the sciatic nerve to the spinal cord where they cross over to the right side and ascend until they stimulate the area for left foot sensation in your right cerebral cortex.
Then, when your cerebral cortex has told you that you’ve been tickled, and if you decide to move your left foot to avoid the tickling, then the motor center that controls the muscles for that action, which are largely contained in the right cerebral motor strip, sends messages back down the spinal cord. But instead of using the sensory “wires”, it sends its messages along the motor “wires”. These messages will pass through the brainstem where they’ll cross over to the left side before winding their way down within the motor nerve section and exiting the spinal cord in a motor nerve root. The messages will continue along various motor neurons on their way to several left leg muscles that will be used to pull away from your tickling tormentor.
But here’s the catch. Even though we know that the nervous system is sending messages to the muscles and is telling them what to do, how are the muscles set up so that they are actually able to do what they’re instructed to do? What else is needed beyond the ability of the motor cortex in the brain to ultimately stimulate a particular muscle to contract, for it to be able to perform any useful work for the body? In other words, just having nerve cells that stimulate and tell muscle cells to contract is not enough to explain how a primitive hominid would be able to run and catch its prey.
Diagnostic Break
Before we begin to answer these questions, I would like to take this opportunity to review my friend’s diagnostic dilemma in regards to what has been stated so far. Specifically, I would like to address the possibility of her having a dysfunction involving either the peripheral nerves or the motor neuron section of the spinal cord. Much of what follows later will involve the coordinated activity of the higher centers of the central nervous system, so I think that now is a good time to consider the possible involvement of the lower motor neuron in my friend’s presenting symptomatology.
The classic example of a condition that affects the peripheral motor nerves, often resulting in a progressive loss of muscle function, is Guillain Barre Syndrome (G.B.S.). This disease usually comes on after an infection, in which inflammation of the peripheral nerves results in injury and dysfunction of the myelin sheath surrounding the axons. (see Wired for Much More than Sound—Neurons and How They Work Part I—The Impulse). You may recall that myelin is important for transmission of the electrical impulse along the nerve and therefore any interference in its structure will often result in an interruption of nerve function. In many ways, G.B.S. is the peripheral nervous system equivalent of Multiple Sclerosis (M.S.).
Usually this condition presents with tingling and weakness in the legs resulting in the inability to walk and stand. This is often followed by a quick progression of nerve dysfunction up the body resulting in difficulty swallowing and breathing. My friend had none of these symptoms. While sitting and standing she had good muscle strength. It appeared that her problem seemed to revolve around changes in position and activities that required high degrees of muscle coordination. So I don’t think that a motor peripheral neuropathy is her problem.
The classic example of a condition that causes damage directly to the motor neuron is Amyotrophic Lateral Sclerosis (A.L.S.) commonly known as Lou Gehrig’s Disease.
This condition involves destruction of the motor neuron within the spinal cord and the brain stem. Its hallmark sign is muscle weakness that can start anywhere in the body that then progresses into other areas. Once again, muscle weakness and atrophy is what is demonstrated on examination and my friend does not have this problem. She is able to stand without difficulty and formal muscle strength examination did not disclose any weakness. So I don’t think that her problem involves a motor neuron disease process.
Back to Basics
Now, let’s look a little closer at exactly how you would achieve the function of pulling your foot away to avoid the tickle monster. If you really think about it, depending on how fast you would want to move your foot away, there would be three separate actions that you could perform. Most of the time you would do all three at once. Try it yourself right now and see. Did you see, or should I say, feel it?
Generally speaking, most people would do a combination of pulling up the thigh (flexing the hip), bending (flexing) the knee, and lifting up the foot (dorsiflexing the ankle). All of these actions, over three separate joints, require the coordinated action of several muscles. But, just as important is the fact that they also move your bones. Do the action again and take note of the muscles that you are using. Now notice the thick bands that you can feel and see in the upper outer thigh, behind the knees and over the top of the feet. These bands are called tendons and without them most muscles would be useless.
As the term denotes, skeletal muscle consists largely of muscles that are attached to the skeleton. The muscles are attached to the bone by these tendons. But each tendon has specialized tissue at each end where it attaches to the bone. One end is called the origin and the other end is called the insertion. The origin of a muscle is usually located along the bone that does not move when the muscle in question contracts. The insertion of a muscle is attached to an adjacent bone in such a manner that when the muscle contracts this bone moves toward the other one and thereby action takes place.
For example, the muscles that allow you to make a fist have their origins along the inner surface of the forearm bones and their insertions span out to the inner surface of the fingers. Likewise, the muscles that allow you to straighten out your fingers have their origins on the outer surface of the forearm bones and their insertions connect up with the fingers on their outer surfaces. Just flex and extend your fingers and you’ll be able to feel the muscle contracting at its origin along both sides of the forearm and you’ll be able to see the tendons at work on both sides of your fingers.
So you can see that having bones in and of themselves would seem to be pretty useless unless you have muscles to be able to move them. And muscles would be pretty useless if they weren’t attached to bones with the specialized connecting tissue called tendons. And by the way, don’t forget that in order for us to be able to walk and run, we need to be able to move our limbs around joints such as the hip, the knee, the ankle, the small joints of the foot, the shoulder, the elbow and the wrist. All of the bones that form these joints are held together by ligaments in order to maintain their integrity and strength.
Now it’s interesting to note from a biomechanical viewpoint that the muscles and their attachments on the bone are ideally suited to perform their jobs. In other words, the origin and the insertion of any given muscle are perfectly situated in a fashion that allows for the most efficient function. And as we mentioned before, the muscles that are needed for strength, such as in the leg, the arm and the back, have enough muscle fibers and nervous control to allow for their heavy and coarse activity. While the smaller muscles that are necessary for finely controlled activities, such as those around the eyeball and the fingers, have just the right amount of nervous control that allows for the precise and delicate movements that are necessarily made by these muscle units.
Partners for Life
But let’s not forget that every bone that moves around a joint often does so in at least three different directions: which requires at least six different muscles to allow for this function. If you consider the shoulder, the wrist, the finger, the hip, the knee and the ankle you will notice that each of these joints can move up and down, in and out and they can also rotate as well. I point this out to show you that, in general, for every skeletal muscle that exists there is an antagonistic, or counteracting, one that has the exact opposite function.
Just like the muscles that flex and extend the fingers, the same applies for the elbow; the biceps muscle flexes it and the triceps muscle extends it; the knee, the quadriceps muscle extends it and the hamstring muscles flex it. Check out all your joints and you’ll see what I’m talking about. What a lot of people don’t realize is that in order for a muscle to be able to contract and move a bone across a joint, it is equally important that its opposing muscle relax so as to allow it to perform this function.
When considering gross actions that simply require the full contraction of one muscle and the full relaxation of its counterpart, such as forcefully flexing your biceps to show how strong you are, or arising from a deep squatting position to a position where your knees are locked in full extension, it may be easy to contemplate how the body is able to perform these “all or nothing” actions.
But consider some alternating movements at first slow and then faster rates, such as opening and closing your fist, turning your wrist over and back, and going up and down on your tiptoes. Go ahead, try it out now. Do each of these movements slowly and then gradually increase the speed to your maximum capacity. Now try it again, but this time try to simulate what it would be like if the complementary muscles that are supposed to be relaxing while the others are contracting are a bit hung up. You should notice that when you try this exercise, some tremor, stiffness, and ultimately, dyscoordination results.
Now think about the finely tuned actions that are necessary for activities such as handwriting, eye movements, speech, and maintaining one’s balance. These actions require very precise and coordinated muscular action. This means that the complementary muscles across one or more joints must be able to work in a coordinated fashion in order for a particular function to take place. I hope this little exercise has demonstrated to you how important it is for the neuromuscular system to be able to coordinate muscle activity in order for our survival on earth.
But how is the neuromuscular system of the body able to perform these feats of precision? To begin to answer these questions, we must first look at the organs of proprioception that inform the central nervous system of what is going on within the muscles and the joints. Only then can we even begin to understand how coordinated muscular activity in the human is even possible, never mind how it came into being. Without considering all of this, it would be like trying to explain the development of the most sophisticated man-made machine without accounting for how it actually works.
What’s Happening Out There?
The proprioceptors are the sensory organs that are located within the muscles, tendons, and joints that provide information to the body about ongoing muscular activity. The main proprioceptors are the muscle spindles and the Golgi tendon organs. The muscle spindles lie within and between the muscles fibers i.e. in parallel, and therefore are sensitive to muscle length and its rate of change. (Figure 2) The Golgi tendon organs lie within the tendon and are in contact with the muscle contractile elements and are therefore sensitive to the tension applied by muscle contraction on the tendon. (Figure 3).
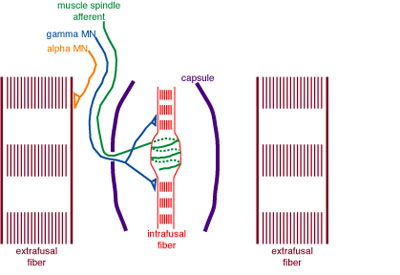
Figure 2. The muscle spindles, with their "intrafusal" fibers, sit between the regular contractile "extrafusal" muscle fibers. The green line is the sensory neuron that sends the messages from the muscle spindle to the spinal cord. The orange line is the motor neuron that tells the extrafusal muscle to contract. The blue line is the neuron that sends messages to the muscle spindle from higher centers.
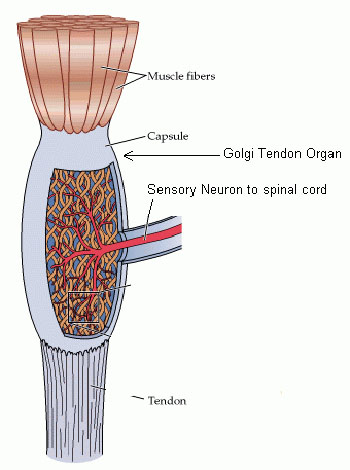
Figure 3. Golgi Tendon Organ.
The information that both the muscle spindles and Golgi tendon organs provide must be integrated by the central nervous system in order to allow for coordinated muscle action. This would have been absolutely necessary for survival of our hominid ancestors. And wonder of wonders, it just so happens that there is a much higher concentration of these sensory organs in the muscles that are necessary for fine motor control. Muscles such as the ones in the hands, the eyes and the neck.
I am unaware of any medical condition that involves either the total absence, or the limited presence, of these proprioceptors within the muscles, tendons and joints. Posture, balance, and coordinated muscular activity, are vitally dependent on these proprioceptors and it is oftentimes the inability of the higher centers of the central nervous system to efficiently integrate the information provided by these sensors that results in loss of balance and dyscoordination. Gravity is a tough taskmaster. You must compensate in time or else you’ll end up right on your gluteus maximus, or worse. So having a basic understanding of how these proprioceptors do their jobs, and the consequences of their activities, is important in order to appreciate neuromuscular function, and parenthetically, to be able to critically assess the validity of what macroevolution teaches about how this system must have come into being.
It’s All in the Reflexes
I’m sure that everyone is familiar with the classic knee-jerk reflex test done by physicians in order to help them assess a patient’s neuromuscular status. But are you aware of the underlying mechanism behind what is actually happening at the neurophysiological level in order to make the results of this test capable of giving physicians reliable information?
By looking at how some of our reflexes work we’ll be able to see how these proprio-ceptors function and thereby get some insight into the true complexity of coordinated neuromuscular activity. And later on, when it is demonstrated how the failing of any one integrating component results in significant neuromuscular dysfunction and debility, which for our hominid ancestors would have spelled certain death, one will readily be able to discern the absolute survival necessity of a fully operational neuromuscular system that defies a step-by-step mechanism of development.
So what exactly is it that makes the knee go into full extension when the patellar tendon of the quadriceps (thigh) muscle is tapped by the examiner? The tapping of the tendon applies a stretch to the quadriceps tendon and this in turn stretches the muscle spindles within it. The muscle spindles always have a certain level of activity that is informing the central nervous system as to the length of the muscles they reside in. But this sudden stretching of the patellar tendon (which is the insertion tendon of the thigh muscle on the foreleg, or tibia bone), further stimulates the muscle spindles and increases their discharges to the spinal cord. Some of these messages continue up the spinal cord to inform the higher centers in the brain, but some of them come in contact with the motor neurons that control the quadriceps. This sudden, maximal increase in stimulation of the muscle spindles due to the quick stretching of the thigh muscle results in the feedback stimulation of the quadriceps to maximally contract and the knee goes into full extension, and woe to the person who is standing in the way (Figure 4).
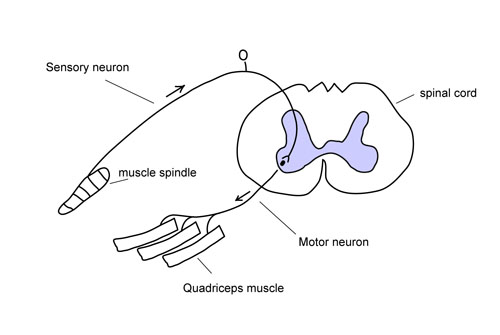
Figure 4. Knee jerk: stretching of patellar tendon stimulates muscle spindles within the quadriceps muscle sending message to the spinal cord and synapsing on the motor neuron that tells the quadriceps muscle to contract and extend the knee: knee jerk..
One could rightly question what the usefulness of such a reflex could be, since the higher centers of the nervous system will eventually be informed of the sudden stretching of the patellar tendon of the quadriceps muscle, and will eventually respond in kind, until one considers how this may affect one’s posture and balance. Timing has everything to do with it. Remember what I stated above; gravity is a tough taskmaster. Time is of the essence. The faster that your neuromuscular system can compensate for an action that may result in you falling on your face, the better for you, and the worse for the plastic surgeon. The point being that a reflexive response to the stretching of the quadriceps tendon by making it contract is always going to be faster than one coming from the brain.
Think of it like being in battle. If the enemy is attacking you and you know that it would be in your best interests to take immediate evasive action, which is more likely to be effective, doing it as soon as you realize that it needs to be done, or waiting until HQ integrates the information and finally gives you the order?
So how does this affect posture? When you are standing upright doing something, you are usually not aware of what your legs are doing because your mind is involved in some other more important activity. You leave it up to your neuromuscular system to keep you where you want to be unless you direct your muscles otherwise. As you continue to stand, your quadriceps muscle tends to fatigue and slacken just a bit, allowing your knee to bend ever so slightly. This mild stretching of the thigh muscle will stretch the muscle spindles within it thereby causing an increase in neural activity going to the spinal cord which will reflexively inform the motor neuron that controls thigh muscle contraction to increase its tone. The resulting increase in contraction of the thigh muscle will almost immediately compensate for the slight slackening that occurred a few milliseconds ago and your posture will be maintained. This is called the tonic-stretch reflex.
One other very important factor is also at play here. Not only do the messages from the muscle spindles come in contact with the motor neurons that control thigh muscle extension activity, but by way of interneurons (interconnecting neurons), they also send inhibitory messages to the motor neurons that control thigh muscle flexion activity, thereby maintaining the proper balance of muscle activity to allow for postural control. This is called reciprocal inhibition.
Now of course, if the quadriceps tendon is contracting too much for a required postural activity, such as standing with the knees partly bent, then the exact opposite will occur.
An increase in contraction of the quadriceps tendon for the posture needed will diminish the output of the muscle spindles which will then decrease their messages to the quadriceps muscle to contract. And the connections to the inhibitory interneurons to the knee flexors would be diminish as well, allowing them to contract a bit more. The overall effect would be a decrease in knee extension and an increase in knee flexion to allow for the required posture of partially bent knees.
On a practical note, the utility of these reflexes can be verified by any person who has ever experienced a dysfunction of the nervous system involving the lower lumbar nerve roots. Control of the quadriceps muscle generally comes from the 3rd and 4th lumbar motor nerve region of the spinal cord. The absence, or diminution of the knee-jerk reflex as compared to the other side, is usually indicative of some sort of pathology involving this area of the spinal cord. The commonest cause would be a slipped intervertebral disc that has shot out laterally from between the spinal bones and is directly pressing on the motor and sensory nerves that are coursing through the nerve root that is forming just outside the spinal cord (Figure 5). Another cause that is often more serious and potentially life-threatening because of what it means systemically, is the direct invasion of metastatic tumor into the L3/4 bone and spinal cord region. These people will tell you that they will be standing somewhere, minding their own business, and suddenly the offending leg will give way and they’ll find themselves on the ground. They may be able to have some measure of control of the leg, depending on how severe their weakness is, but they have to be careful about their posture because they can’t assume that the postural reflexes will kick in automatically. Remember, gravity is a tough taskmaster!! Timing is everything!!
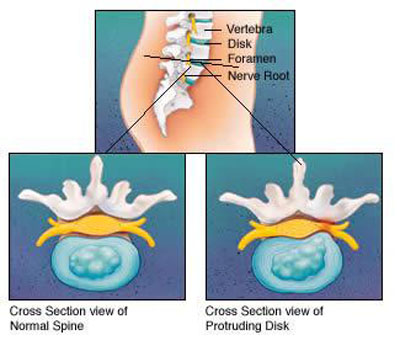
Figure 5. The pressure exerted by the herniated disc on the nerve as shown on the right causes them to dysfunction resulting in sensory and motor consequences.
The Golgi tendon organs play a role in the maintenance of posture as well. The golgi tendon reflex complements and contributes to the actions of the tonic-stretch reflex described above. But, don’t forget that the golgi tendon organs are stimulated by the tension applied by the muscles on the tendons as contraction takes place. Let’s look at the knee again, which is put into extension by the thigh muscles (quadriceps) and into flexion by the hamstring muscles. And remember that when the muscle spindles of the fatiguing quadriceps muscle (the knee extensors) are stimulated by stretching, when the knee begins to flex, by feedback activation, they stimulate it to compensate by increasing its tone, and inhibit, or relax, the hamstrings (knee flexors) to allow the knee to go into more fuller extension to maintain your balance and posture.
When the quadriceps muscle contracts this increases the tension in the patellar tendon which stimulates the Golgi tendon organ. These messages go to the spinal cord and some of them head upward to the higher centers of the nervous system for further interpretation and integration. The remaining messages excite either, interneurons that inhibit quadriceps function (extension of the knee), or interneurons that activate hamstring function (flexion of the knee). i.e. the opposite to what happens with muscle spindle activity (Figure. 6).

Figure 6. Stretching of golgi tendon organ in knee extensor causes inhibition (-) of extensor muscle contraction while stimulating (+) contraction of the knee flexor muscle.
Once again, one must consider how this activity ultimately affects posture. And as you read this, consider the person described above, who has some dysfunction of his L3/4 nerve root, since both the sensory component that carries the messages of the muscle spindles and the Golgi tendon apparatus, and the motor component, which carries the messages for the muscle controlling knee motion, could be similarly affected.
While standing upright, the quadriceps muscle will invariably fatigue and allow some slight flexion at the knee, as described above with regard to muscle spindle activity.
This motion will cause the tension on the patellar tendon to diminish, thereby reducing the neural activity of the Golgi tendon organ within it. This will result in a reduction of the stimulation of the inhibitory interneurons that synapse with the motor neurons of the quadriceps tendon while at the same time diminishing the excitation of the interneurons that stimulate the knee flexors. The combined removal of inhibition of the knee extensors with the reduction of activity to the knee flexors will cause the knee to extend a bit to compensate for the slight flexion that has occurred as noted above in order to maintain posture and balance.
Finally, I am compelled to describe for you the flexion reflex, which is important for one’s ability to quickly withdraw one’s limb(s) from a potentially damaging and noxious stimulus. Above I described what would effectively be going on in your neuromuscular system if your foot were being tickled and then you decided to withdraw it from the tickling. But that decision would have required the time for your brain to interpret and integrate the information that had been received from your foot. What about what happens in the neuromuscular system to protect yourself from limb or life-threatening injury? When you consider how fast you are able to move your limbs to protect yourself, often without you really thinking about it, it would appear that defensive reflexes are in some way playing a part. Here’s what happens.
The reflexive action of limb protection involves multiple levels of sensory and motor activity. Withdrawal of a limb generally involves the flexion of multiple joints as described above. When a noxious stimulus activates the neuromuscular system to go into the protection mode of a particular limb, it activates interneurons that through other ones, both stimulate that limb’s flexors, and inhibit its extensors (Figure.7). In addition, due to what is called the crossed extensor reflex, the limb on the other side will frequently go into extension due to crossing interneurons that stimulate and inhibit the contralateral limbs extensors and flexors respectively. This is thought to help the person to be able to maintain their balance and posture by compensating for what is occurring on the other side of the body.

Figure 7. The flexion reflex and the crossed extensor reflex are shown here: as a painful stimulus sends a message to the spinal cord, it stimulates the flexors of the ipsilateral leg and the extensors of the contralateral leg while inhibiting the extensors of the ipsilateral leg and flexors of the contraleteral leg. The result is that the leg that experiences the painful stimulus withdraws by flexion and the other leg extends in order to maintain balance..
Macroevolution, say what?
In my communications with people who firmly believe in macroevolution, it has always struck me that they seem to hide behind the idea that we are somehow incapable of really knowing what would have been necessary for these hypothetical intermediate systems to function, since we don’t really know what they consisted of in the first place. However, this same position has not in any way deterred them from emphatically stating that these hypothetical intermediate systems must have existed in order for macroevolution to be true, which of course is begging the question. Therefore, this stance would seem to serve only as a defense to their belief based on the convenience of supposed ignorance, and would appear to be an attempt to make the data fit a preconceived theory.
But I would counter that we are certainly capable of applying the knowledge that we have about the human body, with particular attention to the pathophysiology of disease, dysfunction and death, to demonstrate convincingly, that macroevolution, even with the concept of co-evolution, is clearly inadequate to fully explain the complex and interdependent nature of the components that are required for a multi-system organism with a complex body plan to exist on earth. As a case in point, I will mention here what has been discussed so far, and then I will end with a lesson on the underlying neuro-chemistry of coordinated antagonistic muscle function, and a demonstration from medical science of what happens when something in the system goes terribly wrong.
Every bone has specific muscle groups attached to it to allow it to be moved in opposing directions. Which component of each group: flexors/extensors, abductors/adductors, internal rotators/external rotators came into existence first and how did coordinated control that allowed for survival come about? How did the complex sensory structures, known as proprioceptors, which are essentially stretch transducers, come into being? How did they become connected up properly with the central nervous system? And how did the nervous system know what to do with this new sensory information to provide for survival function?
We have already noted that in order for a particular action to take place by the contraction of a specific muscle, it is equally important that its counterpart be able to relax. We have also gone through the exercise of trying to see what it would be like if this did not occur in a coordinated fashion. It gave you an opportunity to mimic the kinds of neurological disorders that we see in healthcare and which we will discuss in next month’s column when we look at the function of the higher centers of the nervous system.
Our understanding of how reflexes work showed that when a message goes out to make a muscle contract, simultaneously, another one is going out to make its counterpart relax, so that coordinated action and survival may occur. Remember that there are many different neurotransmitters and that acetylcholine is the only one used by the motor neurons on muscle tissue. However, the interneurons are the ones that are capable of either stimulating, or inhibiting, motor neuron activity by way of their specific neurotransmitters. So besides having to explain which of the antagonistic muscles around each joint came into existence first, and how a multi-system organism with a complex body plan could have functioned at each step along the way, one would then have to explain how the neuromuscular system, through its various interconnecting neurons, each with its own neurotransmitters, then was able to coordinate the activity of these muscles that allowed for survival.
But in contradiction to the macroevolutionists, who seemingly hide behind this feigned, or otherwise, ignorance of knowing what would have happened without any one component of the neuromuscular system, we do have ample evidence within medical science to prove the point; that macroevolution is poorly qualified to fully explain the development of life. For indeed we do have a medical model that would allow us to appreciate what could happen in a multi-system organism that has the proper set-up of complementary muscles for functional joint activity, but is defective in its ability to allow for proper inhibition of antagonistic muscle action.
One of the main neurotransmitters that is needed for inhibition of muscle activity is glycine. Review of columns I and II on neuromuscular function will remind us that inhibition of nerve function occurs by hyperpolarization of the neuron. This is achieved by the opening of ligand-activated (chemical-activated) Cl- (chloride) ion channels by the attachment of the neurotransmitter, for example, glycine. The opening of Cl- ion channels allows Cl- to go into the neuron and makes the membrane potential more negative, thereby making it more difficult to depolarize, or activate it, thus inhibiting its activity.
Tetanus Anyone?
Let me introduce you to a life-threatening disease called tetanus. This terrible disease was not an uncommon cause of death in the not too distant past. Like rabies, just the thought of it inflicted terror in all of humankind. Watching someone die from tetanus was, and still is, a frightening experience. But with the availability of vaccinations for tetanus, for most of us, this has become only a bad memory in the history of humanity. But what exactly is tetanus and what is the neuropathophysiology behind its deadly effects? Read on and see what life would be like without the neurotransmitter glycine and its capacity for nerve inhibition that allows for proper muscle coordination. It’s not a pretty picture.
Tetanus is a neuromuscular condition brought on by a neurotoxin, called tetanospasmin, that is produced by the anaerobic bacterium called clostridium tetani. It ranks with botulism toxin (see column II of this series, called: The Transfer), as the most potent known microbial toxin. (Rabies is a viral infection of the central nervous system that causes destruction of neural tissue). Tetanus spores are everywhere. In order for tetanus to take hold in someone it usually requires that they suffer a dirty skin injury that is not adequately cleansed and debrided in conjunction with not having adequate immunity to the tetanus toxin.
Tetanospasmin is taken up by the peripheral nerves and is transported slowly backwards to the spinal cord neurons. On reaching the spinal cord, the toxin continues to travel to the region where the neurons that pass impulses coming from the muscle spindles are located. The neurotoxin then blocks the release of neurotransmitters, particularly glycine, which is the main inhibitory neurotransmitter related to coordinated muscular activity. Loss of this inhibition results in uncontrolled and excessive muscle contraction which manifests as severe and often generalized muscle spasms. Even with modern medical techniques, the mortality rate for those who suffer from generalized tetanus is about 25 % and if they survive, it takes about 3 to 6 weeks for a full recovery.
Interestingly enough, strychnine poisoning, which blocks glycine in a similar fashion, often mimicking tetanus, is another medical model that affords us the opportunity to see what it would be like if we didn’t have the neurotransmitter glycine working for us within the neuromuscular system. In one word: dead. And don’t forget that botulism toxin blocks the release of acetylcholine, the absolutely necessary neurotransmitter for motor function, which results in total paralysis, and once again: death. So how did both of these neurotransmitters arrive on the scene and end up right in the right place with the right amount of neural control, and still allow for proper neuromuscular function and survival?
Is it asking too much of those who believe that macroevolution can truly explain the development of all aspects of life, to admit of these glaring weaknesses in their theory, and allow those who are currently being educated to grapple with the controversy?
Or are we continually to be subjected to such mantras as offered to me in a recent e-mail dialogue: “The beauty of the theory of natural selection is that, given enough time, virtually anything that is not an outright violation of the laws of physics, is possible”?
What I have been trying to point out in these columns, which I evidently have failed to impress upon this reader, is the question, not of the outright violations of the laws of physics, but the outright violations of the laws of biological survival, based on our understanding of the pathophysiology of disease, dysfunction, and death.
Future Plans
This column ended up going a bit longer than I expected, but I thought that it was important to give you as much detail as possible in order to understand the complexity of neuromuscular function. Of course you realize that we are only scratching the surface of this incredibly sophisticated system. But I must admit that if you understand what I have written here, then you’ll know this topic as well as I do; which may not be saying very much.
I’ll finish up “Run for Your Life”, and the discussion about what I think may be the cause of my friend’s problems, next month by reviewing what is thought to happen in the higher centers of the central nervous system, in conjunction with our understanding of what happens when they don’t work quite right. It’s sure to illuminate and impress you about the mystery and wonder of life.
After I wrap up with next month’s column, I’ll be taking a break and will likely return in the late spring or early summer with a quarterly column that will begin by touching on some sexually related issues such as; the genetic basis of our sexuality; how Viagra really works; and the pharmacology behind oral contraception and its practical consequences. Of course, tied in with all of the explanations about how these systems work, will be some questions for macroevolution that logically derive from the information presented. Hope to see you then.
Dr. G.
Howard Glicksman M. D. graduated from the University of Toronto in 1978. He practiced primary care medicine for almost 25 yrs in Oakville, Ontario and Spring Hill, Florida. He recently left his private practice and has started to practice palliative medicine for a Hospice organization in his community. He has a special interest in how the ethos of our culture has been influenced by modern science’s understanding and promotion of what it means to be a human being.
Copyright 2005 Dr. Howard Glicksman. All rights reserved. International
copyright secured.
File Date: 4.01.05